Facts About Glaucoma
This information was developed by the National Eye Institute to help patients and their families search for general information about glaucoma. An eye care professional who has examined the patient’s eyes and is familiar with his or her medical history is the best person to answer specific questions.
Glaucoma Defined
How does the optic nerve get damaged by open-angle glaucoma?
Several large studies have shown that eye pressure is a major risk factor for optic nerve damage. In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. (See diagram below.) When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
In open-angle glaucoma, even though the drainage angle is “open”, the fluid passes too slowly through the meshwork drain. Since the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma-and vision loss—may result. That’s why controlling pressure inside the eye is important.
Another risk factor for optic nerve damage relates to blood pressure. Thus, it is important to also make sure that your blood pressure is at a proper level for your body by working with your medical doctor.
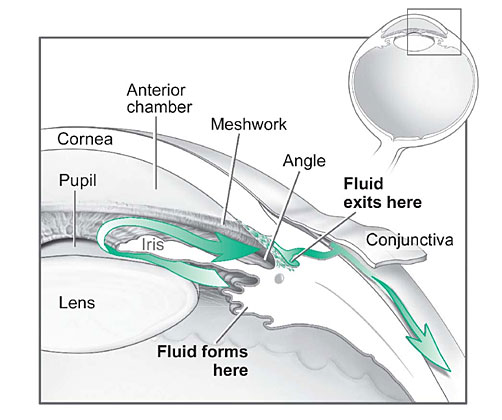
Fluid pathway is shown in teal.
Can I develop glaucoma if I have increased eye pressure?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher levels of eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Can I develop glaucoma without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is a type of open-angle glaucoma.
Who is at risk for open-angle glaucoma?
Anyone can develop glaucoma. Some people, listed below, are at higher risk than others:
African Americans over age 40
Everyone over age 60, especially Mexican Americans
People with a family history of glaucoma
A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eyedrops reduce the risk of developing glaucoma by about half.
Can glaucoma be cured?
No. There is no cure for glaucoma. Vision lost from the disease cannot be restored.
Glaucoma Treatments
Immediate treatment for early-stage, open-angle glaucoma can delay progression of the disease. That’s why early diagnosis is very important.
Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma.
Medicines. Medicines, in the form of eyedrops or pills, are the most common early treatment for glaucoma. Taken regularly, these eyedrops lower eye pressure. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye.
Before you begin glaucoma treatment, tell your eye care professional about other medicines and supplements that you are taking. Sometimes the drops can interfere with the way other medicines work.
Glaucoma medicines need to be taken regularly as directed by your eye care professional. Most people have no problems. However, some medicines can cause headaches or other side effects. For example, drops may cause stinging, burning, and redness in the eyes.
Many medicines are available to treat glaucoma. If you have problems with one medicine, tell your eye care professional. Treatment with a different dose or a new medicine may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take, their medicine. You need to use the drops or pills as long as they help control your eye pressure. Regular use is very important.
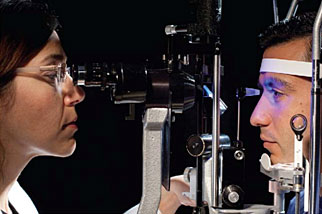
A tonometer measures pressure inside the eye to detect glaucoma.
Make sure your eye care professional shows you how to put the drops into your eye. For tips on using your glaucoma eyedrops, see the inside back cover of this booklet.
Laser trabeculoplasty. Laser trabeculoplasty helps fluid drain out of the eye. Your doctor may suggest this step at any time. In many cases, you will need to keep taking glaucoma medicines after this procedure.
Laser trabeculoplasty is performed in your doctor’s office or eye clinic. Before the surgery, numbing drops are applied to your eye. As you sit facing the laser machine, your doctor holds a special lens to your eye. A high-intensity beam of light is aimed through the lens and reflected onto the meshwork inside your eye. You may see flashes of bright green or red light. The laser makes several evenly spaced burns that stretch the drainage holes in the meshwork. This allows the fluid to drain better.
Like any surgery, laser surgery can cause side effects, such as inflammation. Your doctor may give you some drops to take home for any soreness or inflammation inside the eye. You will need to make several follow-up visits to have your eye pressure and eye monitored.
If you have glaucoma in both eyes, usually only one eye will be treated at a time. Laser treatments for each eye will be scheduled several days to several weeks apart.
Studies show that laser surgery can be very good at reducing the pressure in some patients. However, its effects can wear off over time. Your doctor may suggest further treatment.
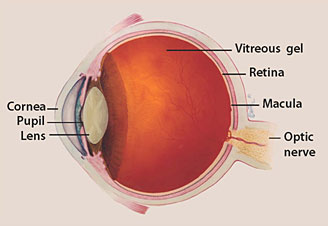
Conventional surgery. Conventional surgery makes a new opening for the fluid to leave the eye. (See diagram on the next page.) Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines and laser surgery have failed to control pressure.
Conventional surgery, called trabeculectomy, is performed in an operating room. Before the surgery, you are given medicine to help you relax. Your doctor makes small injections around the eye to numb it. A small piece of tissue is removed to create a new channel for the fluid to drain from the eye. This fluid will drain between the eye tissue layers and create a blister-like “filtration bleb.”
For several weeks after the surgery, you must put drops in the eye to fight infection and inflammation. These drops will be different from those you may have been using before surgery.
Conventional surgery is performed on one eye at a time. Usually the operations are four to six weeks apart.
Conventional surgery is about 60 to 80 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
Sometimes after conventional surgery, your vision may not be as good as it was before conventional surgery. Conventional surgery can cause side effects, including cataract, problems with the cornea, inflammation, infection inside the eye, or low eye pressure problems. If you have any of these problems, tell your doctor so a treatment plan can be developed.
What are some other forms of glaucoma and how are they treated?
Open-angle glaucoma is the most common form. Some people have other types of the disease.
In low-tension or normal-tension glaucoma, optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures.
A comprehensive medical history is important to identify other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
In angle-closure glaucoma, the fluid at the front of the eye cannot drain through the angle and leave the eye. The angle gets blocked by part of the iris. People with this type of glaucoma may have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately. This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to restore the flow of fluid, the eye can become blind. Usually, prompt laser surgery and medicines can clear the blockage, lower eye pressure, and protect vision.
In congenital glaucoma, children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines are not effective and can cause more serious side effects in infants and be difficult to administer. Surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.

Conventional surgery makes a new opening for the fluid to leave the eye.
Secondary glaucomas can develop as complications of other medical conditions. For example, a severe form of glaucoma is called neovascular glaucoma, and can be a result from poorly controlled diabetes or high blood pressure. Other types of glaucoma sometimes occur with cataract, certain eye tumors, or when the eye is inflamed or irritated by a condition called uveitis. Sometimes glaucoma develops after other eye surgeries or serious eye injuries. Steroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. There are two eye conditions known to cause secondary forms of glaucoma.
Pigmentary glaucoma occurs when pigment from the iris sheds off and blocks the meshwork, slowing fluid drainage.
Pseudoexfoliation glaucoma occurs when extra material is produced and shed off internal eye structures and blocks the meshwork, again slowing fluid drainage.
Depending on the cause of these secondary glaucomas, treatment includes medicines, laser surgery, or conventional or other glaucoma surgery.
What research is being done?
Through studies in the laboratory and with patients, NEI is seeking better ways to detect, treat, and prevent vision loss in people with glaucoma. For example, researchers have discovered genes that could help explain how glaucoma damages the eye.
NEI also is supporting studies to learn more about who is likely to get glaucoma, when to treat people who have increased eye pressure, and which treatment to use first.
What should I ask my eye care professional?
You can protect yourself against vision loss by working in partnership with your eye care professional. Ask questions and get the information you need to take care of yourself and your family.
What are some questions to ask?
About my eye disease or disorder…
What is my diagnosis?
What caused my condition?
Can my condition be treated?
How will this condition affect my vision now and in the future?
Should I watch for any particular symptoms and notify you if they occur?
Should I make any lifestyle changes?
About my treatment…
What is the treatment for my condition?
When will the treatment start and how long will it last?
What are the benefits of this treatment and how successful is it?
What are the risks and side effects associated with this treatment?
Are there foods, medicines, or activities I should avoid while I’m on this treatment?
If my treatment includes taking medicine, what should I do if I miss a dose?
Are other treatments available?
About my tests…
What kinds of tests will I have?
What can I expect to find out from these tests?
When will I know the results?
Do I have to do anything special to prepare for any of the tests?
Do these tests have any side effects or risks?
Will I need more tests later?
Other suggestions
If you don’t understand your eye care professional’s responses, ask questions until you do understand.
Take notes or get a friend or family member to take notes for you. Or, bring a tape recorder to help you remember the discussion.
Ask your eye care professional to write down his or her instructions to you.
Ask your eye care professional for printed material about your condition.
If you still have trouble understanding your eye care professional’s answers, ask where you can go for more information.
Other members of your healthcare team, such as nurses and pharmacists, can be good sources of information. Talk to them, too.
Today, patients take an active role in their health care. Be an active patient about your eye care.
Loss of Vision
If you have lost some sight from glaucoma, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments.
How should I use my glaucoma eyedrops?
If eyedrops have been prescribed for treating your glaucoma, you need to use them properly, as instructed by your eye care professional. Proper use of your glaucoma medication can improve the medicine’s effectiveness and reduce your risk of side effects.
To properly apply your eyedrops, follow these steps:
Wash your hands.
Hold the bottle upside down.
Tilt your head back.
Hold the bottle in one hand and place it as close as possible to the eye.
With the other hand, pull down your lower eyelid. This forms a pocket.
Place the prescribed number of drops into the lower eyelid pocket. If you are using more than one eyedrop, be sure to wait at least 5 minutes before applying the second eyedrop.
Close your eye OR press the lower lid lightly with your finger for at least 1 minute. Either of these steps keeps the drops in the eye and helps prevent the drops from draining into the tear duct, which can increase your risk of side effects.
The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government’s lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.
Glaucoma Defined
What is Glaucoma?
Glaucoma is a group of diseases that damage the eye’s optic nerve and can result in vision loss and blindness. However, with early detection and treatment, you can often protect your eyes against serious vision loss.
The optic nerve
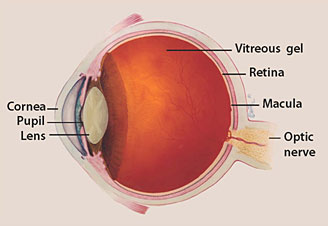
The optic nerve is a bundle of more than 1 million nerve fibers. It connects the retina to the brain. (See diagram above.) The retina is the light-sensitive tissue at the back of the eye. A healthy optic nerve is necessary for good vision.
Glaucoma is a group of diseases that damage the eye’s optic nerve and can result in vision loss and blindness. However, with early detection and treatment, you can often protect your eyes against serious vision loss.
The optic nerve
The optic nerve is a bundle of more than 1 million nerve fibers. It connects the retina to the brain. (See diagram above.) The retina is the light-sensitive tissue at the back of the eye. A healthy optic nerve is necessary for good vision.
How does the optic nerve get damaged by open-angle glaucoma?
Several large studies have shown that eye pressure is a major risk factor for optic nerve damage. In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. (See diagram below.) When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
In open-angle glaucoma, even though the drainage angle is “open”, the fluid passes too slowly through the meshwork drain. Since the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma-and vision loss—may result. That’s why controlling pressure inside the eye is important.
Another risk factor for optic nerve damage relates to blood pressure. Thus, it is important to also make sure that your blood pressure is at a proper level for your body by working with your medical doctor.
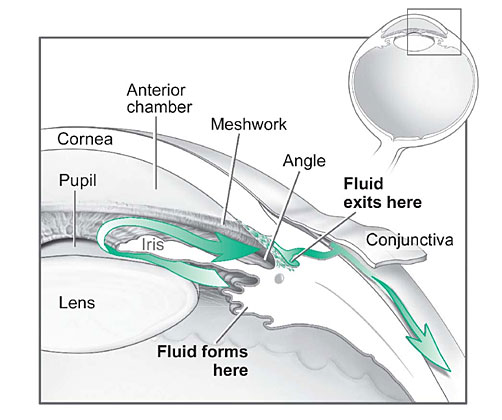
Fluid pathway is shown in teal.
Can I develop glaucoma if I have increased eye pressure?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher levels of eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Can I develop glaucoma without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is a type of open-angle glaucoma.
Who is at risk for open-angle glaucoma?
Anyone can develop glaucoma. Some people, listed below, are at higher risk than others:
African Americans over age 40
Everyone over age 60, especially Mexican Americans
People with a family history of glaucoma
A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eyedrops reduce the risk of developing glaucoma by about half.
Glaucoma Symptoms
At first, open-angle glaucoma has no symptoms. It causes no pain. Vision stays normal. Glaucoma can develop in one or both eyes.
Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. They seem to be looking through a tunnel. Over time, straight-ahead (central) vision may decrease until no vision remains.
At first, open-angle glaucoma has no symptoms. It causes no pain. Vision stays normal. Glaucoma can develop in one or both eyes.
Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. They seem to be looking through a tunnel. Over time, straight-ahead (central) vision may decrease until no vision remains.
How is glaucoma detected?
Glaucoma is detected through a comprehensive dilated eye exam that includes the following:
Visual acuity test. This eye chart test measures how well you see at various distances.
Visual field test. This test measures your peripheral (side vision). It helps your eye care professional tell if you have lost peripheral vision, a sign of glaucoma.
Dilated eye exam. In this exam, drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
Tonometry is the measurement of pressure inside the eye by using an instrument called a tonometer. Numbing drops may be applied to your eye for this test. A tonometer measures pressure inside the eye to detect glaucoma.
Pachymetry is the measurement of the thickness of your cornea. Your eye care professional applies a numbing drop to your eye and uses an ultrasonic wave instrument to measure the thickness of your cornea.
Glaucoma is detected through a comprehensive dilated eye exam that includes the following:
Visual acuity test. This eye chart test measures how well you see at various distances.
Visual field test. This test measures your peripheral (side vision). It helps your eye care professional tell if you have lost peripheral vision, a sign of glaucoma.
Dilated eye exam. In this exam, drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
Tonometry is the measurement of pressure inside the eye by using an instrument called a tonometer. Numbing drops may be applied to your eye for this test. A tonometer measures pressure inside the eye to detect glaucoma.
Pachymetry is the measurement of the thickness of your cornea. Your eye care professional applies a numbing drop to your eye and uses an ultrasonic wave instrument to measure the thickness of your cornea.
Can glaucoma be cured?
No. There is no cure for glaucoma. Vision lost from the disease cannot be restored.
Glaucoma Treatments
Immediate treatment for early-stage, open-angle glaucoma can delay progression of the disease. That’s why early diagnosis is very important.
Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma.
Medicines. Medicines, in the form of eyedrops or pills, are the most common early treatment for glaucoma. Taken regularly, these eyedrops lower eye pressure. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye.
Before you begin glaucoma treatment, tell your eye care professional about other medicines and supplements that you are taking. Sometimes the drops can interfere with the way other medicines work.
Glaucoma medicines need to be taken regularly as directed by your eye care professional. Most people have no problems. However, some medicines can cause headaches or other side effects. For example, drops may cause stinging, burning, and redness in the eyes.
Many medicines are available to treat glaucoma. If you have problems with one medicine, tell your eye care professional. Treatment with a different dose or a new medicine may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take, their medicine. You need to use the drops or pills as long as they help control your eye pressure. Regular use is very important.
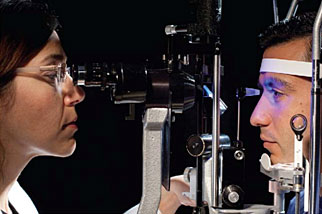
A tonometer measures pressure inside the eye to detect glaucoma.
Make sure your eye care professional shows you how to put the drops into your eye. For tips on using your glaucoma eyedrops, see the inside back cover of this booklet.
Laser trabeculoplasty. Laser trabeculoplasty helps fluid drain out of the eye. Your doctor may suggest this step at any time. In many cases, you will need to keep taking glaucoma medicines after this procedure.
Laser trabeculoplasty is performed in your doctor’s office or eye clinic. Before the surgery, numbing drops are applied to your eye. As you sit facing the laser machine, your doctor holds a special lens to your eye. A high-intensity beam of light is aimed through the lens and reflected onto the meshwork inside your eye. You may see flashes of bright green or red light. The laser makes several evenly spaced burns that stretch the drainage holes in the meshwork. This allows the fluid to drain better.
Like any surgery, laser surgery can cause side effects, such as inflammation. Your doctor may give you some drops to take home for any soreness or inflammation inside the eye. You will need to make several follow-up visits to have your eye pressure and eye monitored.
If you have glaucoma in both eyes, usually only one eye will be treated at a time. Laser treatments for each eye will be scheduled several days to several weeks apart.
Studies show that laser surgery can be very good at reducing the pressure in some patients. However, its effects can wear off over time. Your doctor may suggest further treatment.
Conventional surgery. Conventional surgery makes a new opening for the fluid to leave the eye. (See diagram on the next page.) Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines and laser surgery have failed to control pressure.
Conventional surgery, called trabeculectomy, is performed in an operating room. Before the surgery, you are given medicine to help you relax. Your doctor makes small injections around the eye to numb it. A small piece of tissue is removed to create a new channel for the fluid to drain from the eye. This fluid will drain between the eye tissue layers and create a blister-like “filtration bleb.”
For several weeks after the surgery, you must put drops in the eye to fight infection and inflammation. These drops will be different from those you may have been using before surgery.
Conventional surgery is performed on one eye at a time. Usually the operations are four to six weeks apart.
Conventional surgery is about 60 to 80 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
Sometimes after conventional surgery, your vision may not be as good as it was before conventional surgery. Conventional surgery can cause side effects, including cataract, problems with the cornea, inflammation, infection inside the eye, or low eye pressure problems. If you have any of these problems, tell your doctor so a treatment plan can be developed.
What are some other forms of glaucoma and how are they treated?
Open-angle glaucoma is the most common form. Some people have other types of the disease.
In low-tension or normal-tension glaucoma, optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures.
A comprehensive medical history is important to identify other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
In angle-closure glaucoma, the fluid at the front of the eye cannot drain through the angle and leave the eye. The angle gets blocked by part of the iris. People with this type of glaucoma may have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately. This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to restore the flow of fluid, the eye can become blind. Usually, prompt laser surgery and medicines can clear the blockage, lower eye pressure, and protect vision.
In congenital glaucoma, children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines are not effective and can cause more serious side effects in infants and be difficult to administer. Surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.

Conventional surgery makes a new opening for the fluid to leave the eye.
Secondary glaucomas can develop as complications of other medical conditions. For example, a severe form of glaucoma is called neovascular glaucoma, and can be a result from poorly controlled diabetes or high blood pressure. Other types of glaucoma sometimes occur with cataract, certain eye tumors, or when the eye is inflamed or irritated by a condition called uveitis. Sometimes glaucoma develops after other eye surgeries or serious eye injuries. Steroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. There are two eye conditions known to cause secondary forms of glaucoma.
Pigmentary glaucoma occurs when pigment from the iris sheds off and blocks the meshwork, slowing fluid drainage.
Pseudoexfoliation glaucoma occurs when extra material is produced and shed off internal eye structures and blocks the meshwork, again slowing fluid drainage.
Depending on the cause of these secondary glaucomas, treatment includes medicines, laser surgery, or conventional or other glaucoma surgery.
What research is being done?
Through studies in the laboratory and with patients, NEI is seeking better ways to detect, treat, and prevent vision loss in people with glaucoma. For example, researchers have discovered genes that could help explain how glaucoma damages the eye.
NEI also is supporting studies to learn more about who is likely to get glaucoma, when to treat people who have increased eye pressure, and which treatment to use first.
What You Can Do
If you are being treated for glaucoma, be sure to take your glaucoma medicine every day. See your eye care professional regularly.
You also can help protect the vision of family members and friends who may be at high risk for glaucoma-African Americans over age 40; everyone over age 60, especially Mexican Americans; and people with a family history of the disease. Encourage them to have a comprehensive dilated eye exam at least once every two years. Remember that lowering eye pressure in the early stages of glaucoma slows progression of the disease and helps save vision.
Medicare covers an annual comprehensive dilated eye exam for some people at high risk for glaucoma. These people include those with diabetes, those with a family history of glaucoma, and African Americans age 50 and older.
If you are being treated for glaucoma, be sure to take your glaucoma medicine every day. See your eye care professional regularly.
You also can help protect the vision of family members and friends who may be at high risk for glaucoma-African Americans over age 40; everyone over age 60, especially Mexican Americans; and people with a family history of the disease. Encourage them to have a comprehensive dilated eye exam at least once every two years. Remember that lowering eye pressure in the early stages of glaucoma slows progression of the disease and helps save vision.
Medicare covers an annual comprehensive dilated eye exam for some people at high risk for glaucoma. These people include those with diabetes, those with a family history of glaucoma, and African Americans age 50 and older.
What should I ask my eye care professional?
You can protect yourself against vision loss by working in partnership with your eye care professional. Ask questions and get the information you need to take care of yourself and your family.
What are some questions to ask?
About my eye disease or disorder…
What is my diagnosis?
What caused my condition?
Can my condition be treated?
How will this condition affect my vision now and in the future?
Should I watch for any particular symptoms and notify you if they occur?
Should I make any lifestyle changes?
About my treatment…
What is the treatment for my condition?
When will the treatment start and how long will it last?
What are the benefits of this treatment and how successful is it?
What are the risks and side effects associated with this treatment?
Are there foods, medicines, or activities I should avoid while I’m on this treatment?
If my treatment includes taking medicine, what should I do if I miss a dose?
Are other treatments available?
About my tests…
What kinds of tests will I have?
What can I expect to find out from these tests?
When will I know the results?
Do I have to do anything special to prepare for any of the tests?
Do these tests have any side effects or risks?
Will I need more tests later?
Other suggestions
If you don’t understand your eye care professional’s responses, ask questions until you do understand.
Take notes or get a friend or family member to take notes for you. Or, bring a tape recorder to help you remember the discussion.
Ask your eye care professional to write down his or her instructions to you.
Ask your eye care professional for printed material about your condition.
If you still have trouble understanding your eye care professional’s answers, ask where you can go for more information.
Other members of your healthcare team, such as nurses and pharmacists, can be good sources of information. Talk to them, too.
Today, patients take an active role in their health care. Be an active patient about your eye care.
Loss of Vision
If you have lost some sight from glaucoma, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments.
How should I use my glaucoma eyedrops?
If eyedrops have been prescribed for treating your glaucoma, you need to use them properly, as instructed by your eye care professional. Proper use of your glaucoma medication can improve the medicine’s effectiveness and reduce your risk of side effects.
To properly apply your eyedrops, follow these steps:
Wash your hands.
Hold the bottle upside down.
Tilt your head back.
Hold the bottle in one hand and place it as close as possible to the eye.
With the other hand, pull down your lower eyelid. This forms a pocket.
Place the prescribed number of drops into the lower eyelid pocket. If you are using more than one eyedrop, be sure to wait at least 5 minutes before applying the second eyedrop.
Close your eye OR press the lower lid lightly with your finger for at least 1 minute. Either of these steps keeps the drops in the eye and helps prevent the drops from draining into the tear duct, which can increase your risk of side effects.
The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government’s lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.


Leave a Comment